St Anne’s Academic Review 10 – 2020
What is the Potential for the Use of Complexity Science in the Management of the National Health Service?
Daniel O’Callaghan – Oxford University Centre for the Environment
STAAR 10 – 2020, pp. 46 – 59
——————————–
Published: 01 November 2020
Review process: Open Peer Review
Draft First Uploaded: 01 November 2020. See draft and reviewers’ comments.
Abstract
The United Kingdom’s National Health Service (NHS) is being progressively subjected to greater stress, with pressures caused by changing population dynamics, shifting disease burdens, and economic uncertainty. This has led to a narrative of a ‘NHS in crisis’, with a senior figure in the Care Quality Commission labelling it as a ‘burning platform’ (Wijesuriya et al. 2017). Within this context, complexity theory has been advocated as being able to
improve the NHS’s management. There has been a rapid growth in articles exploring the potential of using complexity science in healthcare systems since the turn of the millennium. However, outside epidemiology, complexity theory has not yet been substantively used in NHS management strategies (Galea et al. 2010). Resultantly, this article explores the possible uses of complexity science in the management of the NHS. It outlines significant possible benefits, while also noting the need for further research to redress current theoretical issues in proposals for its use and to build a more extensive evidence base that would enable complexity science to be incorporated into the management of the NHS.
* * *
Introduction
The NHS is a point of national pride in the UK, aptly demonstrated by the tribute paid towards it in the 2012 Olympics opening ceremony. Recently, the Covid-19 pandemic has placed huge pressure on the NHS. Yet, even prior to Covid-19, there was a narrative of the NHS in distress, with the Red Cross describing aspects of its care provision as a ‘humanitarian crisis’ (Wijesuriya et al. 2017). Additionally, the NHS is becoming increasingly politicised, featuring heavily in general election campaigns, the EU referendum and Brexit negotiations (Hervey and Peers 2016). This narrative of crisis and politicisation has intensified the scrutiny upon the management of the NHS. Whilst the frontline workers are revered, NHS managers have been critiqued and associated with waste and inefficiency (Rimmer 2017). In the face of a growing need to look for new management approaches for the NHS, approaches drawing on complexity science have been advocated as a possible solution. There has been a rapid growth in articles exploring the potential of using complexity science in healthcare systems since the turn of the millennium. However, outside epidemiology, complexity theory has not been substantively used in NHS management strategies (Galea et al. 2010). Indeed, critics state that there is no evidence that complexity science is either needed or would work in health care management (Martin 2018).
This article explores the potential beneficial uses of complexity science in the management of the NHS. Building on this, it identifies the need for further research to redress current theoretical issues in proposals for its use and to build an evidence base that would enable it to be incorporated into the management of the NHS (The Health Foundation 2010). To present this narrative, this article firstly introduces the key features of the NHS as a complex system. It subsequently uses these features to explain current phenomena in the NHS, focusing upon the difficulty of implementing successful, long-term change in the system’s functioning. Following this, it critically analyses current proposals for using complexity science, outlining that whilst promising, they contain a number of theoretical and practical flaws. Finally, it discusses the potential for use of agent-based models in the NHS.
1. The NHS as a Complex System
Complex systems have been identified in diverse domains, from the NHS to shoals of fish (Mitchell 2009). Complex systems are typically identified as those with dynamic interacting components that produce emergent, often self-organising, behaviour (Mitchell 2009). The interactions of complex systems often see them represented as networks, whose topology, type of connections, and node characteristics are crucial to the functioning of the system (Mitchell 2006). Though the NHS is undoubtedly a complex system, the use of complexity science in healthcare systems has been critiqued due to laxity in applying key terms that are defined below (Cairney and Geyer 2017).
2.1. Emergence
Emergence is fundamentally difficult to define precisely (Damper 2000). As Damper (2000) identifies, a ‘neutral’ definition is that large-scale patterns, properties, structures or processes that emerge from interactions within a lower level and with the world that are counter-intuitive or behave in a manner that could not be predicted (Helbing et al. 2011; Krugman 1996; Steels 1991). Therefore, emergence fundamentally relates to new, qualitatively different behaviours at higher levels. Emergence can occur at multiple levels in a complex system such as the NHS, and emergent behaviour at one level can produce emergent behaviour at a higher level (Walloth 2016). For instance, the trends of use of a particular Accident & Emergency (A&E) department is an emergent property of many different individuals’ decisions to visit it whilst nation-wide trends of use for A&E departments is an emergent property of the trends of use of the 181 A&E departments in England (Dattee and Burnham 2010).
2.2. Self-Organisation
Self-organisation refers to the tendency of complex systems to spontaneously order themselves through local interactions without external influence or top-down control, such as the murmuration of starlings in flight (Rickles et al. 2007). A&E departments’ waiting times often exhibit emergent self-organisation (Smethurst and Williams 2002). Self-organised criticality refers to a system that endogenously organises itself close to a critical point (Scheffer et al. 2009). A critical point refers to a point in one or more of the system’s variables beyond which the system’s properties rapidly change as positive feedback loops propel it into a new mode of functioning (Scheffer et al. 2012). Self-organised criticality sees outputs of the system exhibit a power-law distribution. Thus, an input to the system will usually produce a small-scale output; however, it can occasionally lead to a large change in output and change in the system’s functioning (D’Souza 2017). Self-organised criticality has been identified in a number of areas in the NHS system, for instance in waiting times at some hospital departments, and is a crucial factor to appreciate in attempting to change the functioning of the system (Tao and Liu 2015).
2.3. Non-Linearity and Feedback Loops
Integral to both self-organisation and emergent behaviour are non-linear dynamics and feedback loops. Feedback loops refers to an output of an aspect of the system resulting in a new input to the system (Rickles et al. 2007). Feedback loops can act both within and between different scales in the system. Positive feedback loops accelerate change within the system, through a stimulus causing additional change in the same direction. Conversely, negative feedback loops dampen change within the system, where the system reacts to a stimulus by stabilising the systems functioning. It is pertinent to note that both positive and negative feedback loops can be beneficial or detrimental to the system and neither are inherently desirable. Non-linear dynamics simplistically describe a system whose outputs are not proportional to the input, such as in systems that exhibit self-organised criticality (Liu 2007).
2. Complexity as an Explanatory Concept
The dominant reductionist approach to NHS management overlooks the importance of its functioning as a complex system. Reductionist management approaches demarcate the system into ‘manageable’ sub-systems that are perceived to have limited interaction with each other (Plsek and Wilson 2001). For instance, separate budgets and performance targets are set for primary care, secondary care, and social services, with further divisions within these broad units. This division occurs at multiple levels in the NHS, from NHS England to Clinical Commissioning Groups in charge of local areas. Performance targets are set alongside top-down declarations which provide the ‘best’ way to achieve them, often being implemented uniformly despite differing local processes (Chrysanthaki et al. 2013). The logic for this is clear, as it produces ‘simpler’ problems to solve. This reductionist approach builds on the rational planning framework that uses principles of Newtonian science which has guided western management thinking and practice for over a century (Paarlberg and Bielfeld 2009). This approach fundamentally revolves around maintaining organisational stability through developing more rules and adopting more in-depth planning techniques (Paarlberg and Bielfeld 2009). However, this approach creates a bounded rationality and fails to account for the actual functioning of the system (Atun 2012). This inhibits the collaboration advocated for by the principles of the NHS (2017) and fails to consider the importance of emergence in complex systems.
Recognising the possibility for emergent behaviour is crucial in the management of the NHS. Though emergent behaviour is by its nature difficult to predict, failing to consider its occurrence leads to significant issues. Emergent behaviours can be desirable; however, they often lead to policy interventions having significantly different impacts than their stated aims, for instance in hospital waiting times. Hospital waiting times in the NHS exhibit emergent self-organisation, with certain departments displaying self-organised criticality (Love and Burton 2005). Thus, though hospitals with long waiting times often receive focused investment, particularly in A&E departments, they rarely exhibit large scale reductions over the long-term (Smethurst and Williams 2002). Complexity theory is useful in explaining this phenomenon and suggesting more effective strategies to enact systemic change. It is key to note two aspects: firstly, that the trends of a hospitals use are an emergent phenomenon based on the decisions of many individuals: and secondly, that hospitals do not exist in isolation, but are part of a wider network of care provision (Dattee and Burnham 2010). Therefore, this emergent property is an outcome of both internal interactions in the care provision system and this system’s interaction with the world.
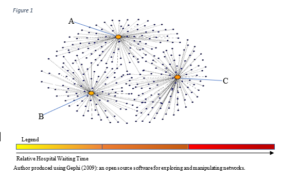
Hospital waiting times can be affected by various factors and have complex feedback loops. There are multiple influences upon an individual’s hospital choice. For instance, the agent-based model developed by Tao and Liu (2015) found that a feedback loop exists between hospital performance and the individual’s selection. A high performing hospital is more likely to have individuals choose to visit it, based upon their own experience and the knowledge gained from the number of networks they interact with (Tao and Liu 2015). This finding has important implications as a hospital is part of a wider system. For instance, consider 3 hospitals, A, B, and C in Figure 1 that serve a spatially bounded area. These hospitals all have similar waiting times and performance measures, and thus individuals when deciding which hospital to visit usually make their decisions based on proximity.
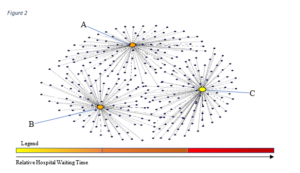
The reductionist management strategy considers hospitals as isolated, and concentrates resources on a single hospital, for instance hospital C. Hospital C receives increased investment, resulting in a reduction in its waiting times (Figure 2). This often results in the initial investment being seen as successful, causing investment to be decreased and the focus to shift to elsewhere in the system (Love and Burton 2005).
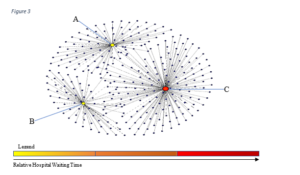
A negative feedback loop emerges, whereby due to personal experience and the knowledge gained from a number of networks, individuals begin to change their decision-making process and are more likely to travel to hospital C than to hospitals A or B due to the reduction in its waiting time. Therefore, hospital C experiences a spike in visitors and can see its waiting times increase above the level they were at prior to the investment as displayed in Figure 3 (Smethurst and Williams 2002).
This eventually leads to a further negative feedback loop whereby individuals begin to choose to travel to hospitals A and B again, thus restoring the distribution of patients to a similar level as prior to the investment (Figure 1). Thus, there is a limited reduction in waiting times as the effects of the investment are dissipated throughout the whole system as it self-organises. This is compounded through interactions with other levels in the NHS. For instance, general practitioners (GP) are more likely to refer individuals to hospital if the waiting times are lower (Love and Burton 2005). Thus, when a hospital’s waiting time decreases, there is an increase in the number of referrals from the GPs and creating another feedback loop. This example demonstrates micro and meso-level interactions producing self-organising emergent behaviour that negates the effect of the investment which is dissipated into the wider network (Smethurst and Williams 2001).
This simple conceptual example demonstrates the necessity of considering the NHS as a complex system due to the effect of feedback loops, interactions and emergence on its functioning. Further, it is crucial to note the importance of temporal scale in the system’s functioning following the investment. The NHS is a complex adaptive system whose structure and behaviour changes over time (Anderson et al. 2003). The inherent inertia and intricate connections across the network inevitably lead to delays in changes in the functioning of the NHS following interventions (Dattee and Barlow 2010). The system’s adaptation over time can lead to policies being implemented, deemed successful after initial positive measures, and then ignored. This is evident in hospital waiting times that are temporarily reduced following investment, before eventually returning to a level similar to where they stood prior to the investment (Smethurst and Williams 2002). Moreover, overlooking temporal lags in the system’s behaviour following policy interjections can lead to corrective actions being taken that can undermine ongoing processes (Dattee and Barlow 2010). This is particularly problematic given the political pressure on governments to produce measurable, quantitative, and rapid success rather than considering the long-term evolution of the system (Sturmberg et al. 2014). Complexity science is a valuable tool to identify the existence of these issues and analyse their effects. Recognising the difficulty in attempting to control a complex system is key to complexity scientists’ proposals for changes in the NHS management structure.
4. Approaching the NHS as a Complex System
The early proposals for the use of complexity sciences in the NHS directly challenge reductionist management strategies and were arguably designed to incite debate rather than to be implemented (e.g. Plsek et al. 2001). Recognising the issues with restrictive top-down control, propositions advocated for control to be reduced to ‘minimum specifications’, arguing that policymakers ‘must give up notions of control over processes of change’ (Best et al. 2012 pp. 423). Minimum specifications involve goals and resources being pooled for each level of the NHS rather than allocated to different subsections. This would facilitate local interactions which can produce innovative emergent behaviours that result in more efficient system functioning (Greenhalgh et al. 2010).
The logic behind ‘minimum specifications’ is clear, as whole system targets could feasibly facilitate interactions that were previously constrained. Indeed, such approaches have dominated in small entrepreneurial organisations, though they have been critiqued for their unpredictability which raises considerable issues for large organisations such as the NHS that require stability (Paarlberg and Biefeld 2009). These radical proposals overlook important aspects of complex systems. Complexity science emphasises that the learnt behaviour of agents has developed over multiple iterations and is resistant to change (Chrysanthaki et al. 2013). Indeed, the competition over performance targets and funding over successive years has led to a ‘blame culture’ between different areas of the NHS (Dattee and Burnham 2010) but to propose that pooling budgets will quickly see the emergence of desirable system-wide behaviour ignores the learnt behaviour of individuals and institutions in the NHS. The proposals assume individuals and institutions in the NHS to be perfectly rational in their behaviour, which is contrary to intuitive understandings of human behaviour and has been robustly rejected by complexity scientists (Beinhocker 2010).
The temporal lag in delivering positive behaviours makes proposals such as that of minimum specifications unsuitable for governments to implement. Furthermore, these proposals tend to conflate the levels of analysis in the NHS (Dattee and Burnham
2010). Desirable emergent behaviours at the scale being observed may be undermining processes at different levels due to interactions between levels that are ignored by focusing upon a particular level of analysis (Lanham et al. 2013). For instance, in minimum specifications, the flexibility may allow GPs to improve their functioning by streamlining the process of referring individuals to hospital. Thus, focusing upon the local level of the GPs indicates a more effective system. However, this fails to consider that this process can change the trends of hospital use, undermining the care provided by hospitals. The issues in such proposals illustrate that the potential of complexity science is not realised through radical approaches. However, complexity science has significant potential in shifting away from reductionist approaches to flexible forms of top-down control.
Complexity science can aid top-down control through providing managers and policymakers at all levels of the NHS with an awareness of its behaviours as a complex system. Lack of appreciation of complex interconnections in the NHS leads to dysfunctional behaviours from policymakers regardless of their intentions (Rouse 2008). Managers with an understanding of complexity theory are more able to recognise and appreciate the interplay between different scales, non-linearity, feedback loops and emergence within the NHS (Rusoja et al. 2018). Further, they are more likely to embrace flexibility by not planning based on the assumptions of predictability and to accept that there is a range of possible outcomes to interventions that can change over time (Lanham et al. 2013). Education is crucial to enabling flexibility in NHS management without reverting to impractical and theoretically questionable minimum specifications. Though the use of this complexity science has been limited in healthcare systems, Brainard and Hunter (2016) found that the majority of interventions using it have achieved positive results. However, their sample size was limited to 29 interventions restricting the ability to draw generalisations. Thus, it is crucial for further research to identify the potential of complexity science in NHS management, similarly to Dattee and Barlow’s (2010) investigation into the 2004 Unscheduled Care Collaborative Program.
The Unscheduled Care Collaborative Program (UCCP) deployed in 2004 exemplifies the benefits of taking an approach that uses complexity science at all levels (Dattee and Barlow 2010). The UCCP successfully reduced the waiting times for access to emergency care in Scotland. Managers worked alongside complexity scientists to identify that waiting times in hospitals across Scotland were in a state of self-organised criticality, with attempts to reduce waiting times resulting in changes that followed a power-law distribution (ibid). Therefore, small changes to key variables can lead to a critical transition in the system’s functioning. This approach led managers to focus on identifying leverage points throughout the system, rather than solely focusing upon individual ‘problem’ hospitals or departments within hospitals. For instance, they produced flow models of patients throughout the system to identify the key points of delay. This allowed them to effectuate change that can be enhanced through positive
feedback as the system passes through a critical transition, rather than being dampened by negative feedback (Hawe 2015). However, managers at local levels found it difficult to identify key leverage points in the system and discern the individual causation of the changes in waiting times (Dattee and Barlow 2010).
The success of UCCP demonstrates the value of incorporating complex systems thinking into all levels of management. It identifies the importance of having knowledge of the entire functioning of the system, rather than of a particular level or section. Local managers’ struggle to identify the system’s leverage points indicates the need for methods to establish different complex, non-linear interactions and feedback loops (Dattee and Barlow 2010). This issue is compounded by the linear models currently employed by NHS managers that rule out these factors. Thus, this indicates the need for models better suited to exploring the mechanisms of the NHS and considering how they may develop over time. In this role, the development of agent-based models could be integral for the use of complexity science in the NHS.
3. Modelling the NHS: Agent-Based Models
The NHS has been extensively modelled throughout its existence, predominantly using linear approaches such as decision trees and Markov models (Marshall et al. 2015). Linear models are limited; they do not consider the possibility of emergence, non-linear dynamics, multiple feedback loops or multiple states of equilibrium that occur in the NHS (Sarriot and Koutletio 2015). Agent-base models (hereafter ABMs) provide the ability to model these attributes of the NHS. Though their use in healthcare systems has been limited, they have been used widely to model social systems, from academic collaboration networks to economic trends (Tomasello et al. 2017). ABMs consist of a number of agents, ranging from individuals to large institutions, that interact with each other. These agents are affected by and can affect the environment of the model. Each agent in these models acts based on a set of internalised rules which can be heterogeneously distributed to agents in the model. Agents can either have fixed rules, or they may be able to adapt their rules and their behaviour over time, thus resulting in adaptation in agents’ interactions, the environment of the model and its output (Bruch and Atwell 2013).
The local interactions between heterogeneous agents in ABMs enable them to model emergent phenomena and the model’s dynamism also allows it to explore changes in the system’s functioning over time (Turrell 2016). The heterogeneity of the agents, alongside the potential for non-linearity and feedback loops, allows ABMs to model more realistic behaviour than traditional linear models (Bruch and Atwell 2013). This ability can allow ABMs to be used as ‘low-risk and low-cost laboratories’ in order to develop a greater understanding of the system and its mechanisms (Marshall et al. 2015). This is crucial, as knowledge of the system’s intrinsic structure is vital in attempting to direct its change (Dattee and Barlow 2010). Managers and policymakers can use ABMs to explore multiple possible outcomes of a prospective policy and develop an awareness of the potential emergent behaviours that can arise from interventions. The value of this has already been demonstrated in healthcare systems. For instance, Megiddo et al. (2016) developed an ABM to test three different initiatives to treat epilepsy in India. This ABM identified that emergent processes that developed over time in one initiative would entail a much higher ongoing financial investment. Thus, policymakers were able to dismiss one of the initiatives based upon the ABM’s results (Megiddo et al. 2016). Further, by running ABMs with a number of different combinations of rules and behaviours, key variables and leverage points for enacting systemic change can be determined (Peters 2014). Thus, an ABM could have proved valuable for managers in the aforementioned UCCP, who were struggling to identify the system’s leverage points. Despite the substantial potential of ABMs, there is resistance to their usage in the management of the NHS.
ABMs are an advance upon existing linear approaches to modelling the NHS: however, they do not have the ability to reliably and accurately predict the outcome of management decisions on the system’s functioning. For instance, whilst the ABM developed by Megiddo et al. (2016) allowed the rejection of one initiative, it was unable to identify which of the other two initiatives would be most effective. The ability to model heterogeneous agents provides modellers with significant freedom in choice (Bruch and Atwell 2013). Though this allows them to model a wide array of phenomena, modellers face difficulty in selecting the correct variables to classify their agents and their behaviour. This can significantly affect the results of the model. For instance, two ABMs of a particular phenomenon can differ markedly based upon the modeller’s choices. Further, regardless of the assumptions made, the non-linearity in the model can lead to the same ABM producing different outcomes in concurrent runs (Turrell 2016). This causes issues in interpreting and using their outputs, which is compounded by the inaccessibility of the models’ underlying code for policymakers leading to criticisms of a lack of transparency (Marshall et al. 2015).
These issues can be partially alleviated by engaging managers throughout the modelling process and educating managers in complexity science to make them more accepting of the multiple potential outputs in the models. The value of ABMs does not lie in their ability to accurately and precisely model all aspects of the system and predict its future functioning. Rather, ABMs’ value is their potential to allow policymakers and managers to experiment with management decisions, explore their potential results and acquire a greater knowledge of the system’s functions. In the context of the NHS, this has the potential to support more accurate, efficient and flexible management (Marshall et al. 2015).
Conclusion
The management of the NHS is being increasingly scrutinised with fears of a collapse and a shift towards a privatized healthcare system (Campbell 2016). It is vital that privatisation is not the solution to the management problems faced by the NHS. Though the NHS has substantive shortcomings, its provision of universal healthcare that is free at the point of access is invaluable. It is important to note that whilst complexity science has significant, compelling value, it is not a panacea for the issues in the NHS. However, it is clear that its potential should not be ignored. Though critics argue that there is little evidence of its benefits, it provides a valuable analytical lens that can be utilised to explain phenomena and structures in the NHS that defy conventional approaches (Martin 2018). Moreover, its use can be extended beyond that of an explanatory concept. Engaging with and educating managers at all levels of the NHS can produce individuals that are adept at grasping the inherent unpredictability of policies, as well as the non-linearity, feedback loops, and emergent phenomena that characterise the system. Thus, they are better equipped to attempt to enact change within the NHS. Moreover, the use of ABMs can provide managers with better knowledge of its underlying mechanisms (Marshall et al. 2015). To realise its potential, complexity scientists need to engage more substantively with practical management proposals, and their proposals and insights should be encouraged and considered by policymakers.
Oxford University Centre for the Environment
Bibliography
Anderson, R. A., Issel, L. M. and McDaniel Jr, R. R. (2003) ‘Nursing homes as complex adaptive systems: relationship between management practice and resident outcomes.’, Nursing research, 52(1), pp. 12–21.
Atun, R. (2012) ‘Health systems, systems thinking and innovation’, Health Policy and Planning. Beinhocker, E. D. (2010) ‘Evolution as Computation : Implications for Economic Theory and Ontology’, Evolution, (2004), pp. 1–30.
Best, A. et al. (2012) ‘Large-system transformation in health care: A realist review’, Milbank Quarterly, pp. 421–456.
Brainard, J. and Hunter, P. R. (2016) ‘Do complexity-informed health interventions work? A scoping review’, Implementation Science.
Bruch, E. and Atwell, J. (2013) ‘Agent-Based Models in Empirical Social Research’, Sociological Methods & Research, 00(0), pp. 1–36.
Cairney, P. and Geyer, R. (2017) ‘a Critical Discussion of Complexity Theory: How Does “Complexity Thinking” Improve Our Understanding of Politics and Policymaking?’, Complexity, Governance & Networks, 3(2), pp. 1–11.
Campbell, D. (2016) How much is the government really privatising the NHS? The Guardian [online] Available at:
https://www.theguardian.com/society/2016/aug/15/creeping-privatisation-nhs-offici al-data-owen-smith-outsourcing [Accessed: 10/10/2017].
Cepoiu-Martin, M. and Bischak, D. P. (2017) ‘Policy choices in dementia care-An exploratory analysis of the Alberta continuing care system (ACCS) using system dynamics’, Journal of Evaluation in Clinical Practice.
Chrysanthaki, T., Hendy, J. and Barlow, J. (2013) ‘Stimulating whole system redesign: Lessons from an organizational analysis of the Whole System Demonstrator programme’, Journal of Health Services Research & Policy, 18(1), pp. 47–55.
D’Souza, R. M. (2017) ‘Curtailing cascading failures’, Science, pp. 860–861.
Damper, R.I., (2000), Editorial for the Special Issue on `Emergent Properties of Complex Systems’ Emergence and levels of abstraction, International Journal of Systems Science, Volume 31, number 7, pages 811 – 818.
Dattée, B. and Barlow, J. (2010) ‘Complexity and whole-system change programmes’, Journal of Health Services Research and Policy, 15(SUPPL. 2), pp. 19–25.
Galea, S., Riddle, M. and Kaplan, G. A. (2010) ‘Causal thinking and complex system approaches in epidemiology’, International Journal of Epidemiology, 39(1), pp. 97–106. Greenhalgh,
T. et al. (2010) ‘Response to “The Appropriation of Complexity Theory in Health Care”’, Journal of Health Services Research & Policy, 15(2), pp. 115–117.
Hawe, P. (2015) ‘Lessons from Complex Interventions to Improve Health’, Annual Review of Public Health, 36(1), pp. 307–323.
Hawking, S. (2000) What is complexity?, Washington Center for Complexity & Public Policy. # Available at: www.complexsys.org.
The Health Foundation (2010) Evidence Scan: Complex adaptive systems. Available online at https://www.health.org.uk/sites/health/files/ComplexAdaptiveSystems.pdf [Accessed 11/04/2018].
Helbing, D., Yu, W. and Rauhut, H. (2011) ‘Self-Organization and Emergence in Social Systems: Modeling the Coevolution of Social Environments and Cooperative Behavior’, The Journal of Mathematical Sociology, 35, pp. 177–208.
Hervey, T. and Peers, S. (2016) ‘Brexit and health services’, Clinical Medicine, Journal of the Royal College of Physicians of London, pp. 101–102. doi: 10.7861/clinmedicine.16-2-101.
Krugman, P. (1996) The Self-organizing Economy. Oxford: Blackwell.
Lanham, H. J. et al. (2013) ‘How complexity science can inform scale-up and spread in health care: Understanding the role of self-organization in variation across local contexts’,
Social Science and Medicine, 93, pp. 194–202. Liu, J. et al. (2007) ‘Complexity of coupled human and natural systems’, Science, pp. 1513–1516.
Love, T. and Burton, C. (2005) ‘General practice as a complex system: A novel analysis of consultation data’, Family Practice, 22(3), pp. 347–352.
Marjanovic, S. Sim, M. Dubow, T. Corbett, J. Harte, Parks, S. Miani, C. Chataway, J. Ling, T. (2017) Innovation as a driver of quality and productivity in UK healthcare: Creating and connecting receptive places. Santa Monica, CA: RAND Corporation, 2017.
Marshall, D. A. et al. (2015) ‘Transforming Healthcare Delivery: Integrating Dynamic Simulation
Modelling and Big Data in Health Economics and Outcomes Research’, PharmacoEconomics, pp. 1–12.
Martin, C. (2018) Complex adaptive systems approaches in health care- A slow but real emergence? Journal of Evaluation in Clinical Practice. 24(1), pp. 266-268.
Megiddo, I. et al. (2016) ‘Health and economic benefits of public financing of epilepsy treatment in India: An agent-based simulation model’, Epilepsia, 57(3), pp. 464–474. Mitchell, M. (2006) ‘Complex systems: Network thinking’, Artificial Intelligence, pp. 1194–1212.
NHS (2013) The principles and values of the NHS in England – NHS Choices, NHS Direct.
Available at: http://www.nhs.uk/NHSEngland/thenhs/about/Pages/nhscoreprinciples.aspx.
Paarlberg and Bielefeld (2009) Complexity Science—An Alternative Framework for Understanding Strategic Management in Public Serving Organizations, International Public Management Journal, 12:2, 236-260.
Peters, D. H. (2014) ‘The application of systems thinking in health: Why use systems thinking?’, Health Research Policy and Systems.
Plsek, P. E. and Wilson, T. (2001) ‘Complexity science: Complexity, leadership, and management
in healthcare organisations’, BMJ, 323(7315), pp. 746–749.
Rickles, D., Hawe, P. and Shiell, A. (2007) ‘A simple guide to chaos and complexity’, Journal of Epidemiology & Community Health, 61(11), pp. 933–937.
Rouse, W. B. (2008) ‘Health Care as a Complex Adaptive System : Implications for Design and Management’, Organization Science, 38(1), p. 17.
Rusoja, E. Haynie, D. Sievers, J. Mustafee, N. Nelson, F. Reynolds, M. Sarriot, E. Swanson, RC. Williams, B. (2018) Thinking about complexity in health: A systematic review of the key systems thinking and complexity ideas in health. Journal of Evaluation in Clinical Practice.
Sarriot, E. and Kouletio, M. (2015) ‘Community health systems as complex adaptive systems: Ontology and praxis lessons from an urban health experience with demonstrated sustainability’, Systemic Practice and Action Research, 28(3), pp. 255–272.
Silverman, E., Gostoli, U., Picascia, S., Almagor, J., McCann, M., Shaw, R. and Angione, C., 2020.
Situating Agent-Based Modelling in Population Health Research.
Smethurst, D. P. and Williams, H. C. (2002) ‘Self-regulation in hospital waiting lists’, Journal of the Royal Society of Medicine, 95(6), pp. 287–289.
Steels, L., 1991, Towards a theory of emergent functionality in Meyer, J and Wilson, S From Animals to Animats, Proceedings of the First International Conference on Simulation of Adaptive Behavior Cambridge, MA : MIT press, pp. 451-461.
Sturmberg, J. P., Martin, C. M. and Katerndahl, D. A. (2014) ‘Systems and complexity thinking in
the general practice literature: An integrative, historical narrative review’, Annals of Family Medicine, pp. 66–74.
Tao, L. and Liu, J. (2015) ‘Understanding self-organized regularities in healthcare services based on autonomy oriented modeling’, Natural Computing, 14(1), pp. 7–24.
Tomasello, M. V., Vaccario, G. and Schweitzer, F. (2017) ‘Data-driven modeling of collaboration networks: a cross-domain analysis’, EPJ Data Science, 6(1).
Turrell, A. (2016) ‘Agent-based models : understanding the economy from the bottom up’, Quarterly Bulletin of the Bank of England, Q4(1), pp. 173–188.
Walloth, C. (2016) Emergent Nested Systems: A Theory of Understanding and Influencing Complex Systems as well as Case Studies in Urban Systems. Cham: Springer.
Wijesuriya, J., White, B. and Modi, N. (2017) ‘Response to Offline: Is the NHS in crisis?’, The Lancet V390 p. 225.

What is the Potential for the Use of Complexity Science in the Management of the National Health Service? by Daniel O’Callaghan is licensed under a Creative Commons Attribution 4.0 International License.
<< Back to Contents
<< Back to Publications
St Anne's Academic Review (STAAR) A Publication by St Anne's College Middle Common Room ISSN 2048-2566 (Online) ISSN 2515-6527 (Print)
